28 May FODMAPS and Irritable Bowel
Cranky guts
We’ve all had tummy trouble at one time or another but as of 2012 nearly 20% of the population could be aptly diagnosed with Irritable Bowel Syndrome and 1.35 billion dollars was spent that year on the condition in the U.S. (Magge & Lembo, 2012). The standard American diet is perfectly suited to reducing immunity, degrading epithelial cell walls and promoting dysbiosis….so that’s awesome. I get questions ALL the time about gut health, which is good since it’s my specialty, so for this blog I thought I’d focus on teaching a little bit about how FODMAP’s, probiotics and prebiotics affect inflammatory bowel diseases.
IBS
Irritable bowel symptoms vary from abdominal pain, altered bowel function and dyspepsia to anxiety and depression (Pizzorno, Murray, & Joiner-Bey, 2016). While many therapeutic options are relevant in the integrative approach (addressing food intolerance, stress, sleep etc) something that gets brought up a lot is a low FODMAP diet to manage symptoms and heal the gut for clients with IBS.
FODMAPS
FODMAP’s (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) are short-chain carbohydrates that are osmotically active and produce hydrogen / carbon dioxide when fermented by intestinal bacteria (Pizzorno, Murray, & Joiner-Bey, 2016). The production of these gases increases bloating and distension can also be related to water retention, especially in the small intestinal lumen, resulting from the osmotic effects of slow, small molecule absorption (Muir & Gibson, 2012). While the pathology of Irritable Bowel Syndrome isn’t fully understood, FODMAP’s can contribute to the visceral hypersensitivity, altered motility, abnormal colonic fermentation, and sugar malabsorption, which are usually present in IBS patients (Magge & Lembo, 2012).
Good vs Bad Bugs
Because many people with IBS may be suffering from dysbiosis of the gut microbiota, including location and variety of bacteria, increasing microbiome health is relevant for IBS patients. Increasing microbiome diversity can be an effective treatment, along with supplements anda a low FODMAP diet, in preventing flares and improving gut health (Muir & Gibson, 2013). The chronic inflammation, that is in part due to harmful microbiota, made me curious as to how much research has been done with probiotics and IBD (Lee et al, 2014).
Have you tried to “fix” your IBS and felt worse?
While simulating indigenous bacteria sounds like it would have a positive effect on bacterial imbalance, the research I found showed that the results were incredibility varied because many participants had to pull out of studies due to bloating and discomfort (Lee et al, 2014). This is why individualized nutritional counseling is so integral to success for clients!!! No two people are the same! Using strategic medicine, as Dr. Ben Lynch calls it, I can narrow down the therapeutic options to the interventions that are most likely to succeed and then use a little bit of trial and error to find the perfect diet and supplementation for each person so that they can thrive and not just survive
Don’t go away empty handed
Here’s a freebie for you if you want to do something TODAY to start feeling better:
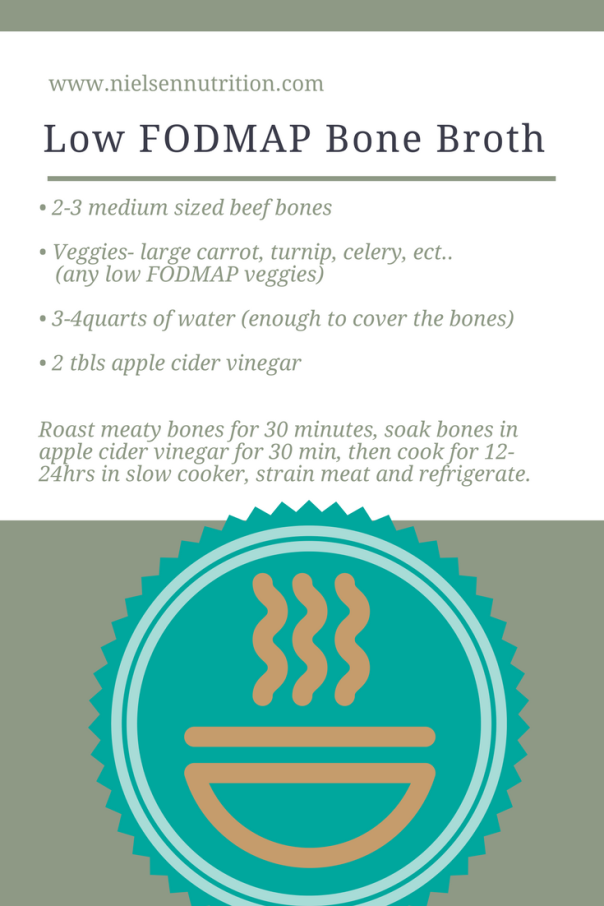
While bone broth is usually my go to recommendation for digestive distress I had to think a little harder when I realized that the typical main ingredients I like to use (onion and garlic) are not on the approved list of low FODMAP foods. Luckily you can still make a nutrient dense stock rich in glutamine and low in FODMAP’s by using this recipe.


Sorry, the comment form is closed at this time.